Endoprosthesis implants stand out as one of the prevailing medical interventions among individuals aged 65 and older [1]. Given the frequency of these procedures, our understanding of potential complications has substantially progressed. Foremost among these complications is periprosthetic joint infection (PJI), a significant concern despite its relatively low occurrence (approximately 1.5% of patients experience PJI during the decade after surgery) [2, 3]. PJI remains a leading contributor to artificial joint dysfunction, often necessitating repeat arthroplasty and thereby influencing perioperative risks and incurring avoidable costs [4].
The multifactorial nature of PJI incidence underscores the importance of investigating causative factors. Dentoalveolar infections and poor dentition have emerged as an area of interest for clinicians, presenting a theoretical avenue for prevention through preoperative dental assessment (PDA) and targeted treatment of infection sources [2]. However, currently, there are no guidelines that suggest a specific dental approach to reduce incidence of PJI: 1) recommendations of the European Knee Associates, International Committee American Association of Hip and Knee Surgeons and Arthroplasty Society in Asia based on a survey of members do not mention any dental intervention as a preoperative measure of prevention of PJI [5]; 2) the American Academy of Orthopaedic Surgeons in its guidelines published in 2019 stated that there is insufficient evidence that poor dental status increases the risk for PJI [6]; and 3) in the guidelines published in 2018 in “Current Reviews in Musculoskeletal Medicine” the authors recommended following ‘a common-sense approach’, suggesting performing dental exa-mination and clearance on patients with evidence of existing dental pathology [7]. Despite those opi-nions, obligatory dental clearance remains a common approach [8–10]. Recent data based on a representative sample from Polish orthopaedic units show that obligatory dental clearance is requested by 40% of physicians prior to the surgery [11], while 60% do not follow such an approach.
Given this context, our meta-analysis aimed to assess the data on the consequences of PDA in averting PJI incidents. This intervention specifically targeted patients undergoing total joint arthroplasty (TJA). By synthesizing relevant studies, our aim was to provide a summary of what is known about the consequences of incorporating preoperative dental measures into the broader framework of joint replacement procedures.
METHODS
The protocol for this systematic review was registered at the international prospective register of systematic reviews (PROSPERO: CRD42023458210). The PRISMA checklist was implemented for appropriate reporting in this work [12].
Eligibility criteria
Any studies were eligible for inclusion if they were conducted in line with the PICO assumptions: population (P): adult patients undergoing TJA; intervention (I): PDA (dental assessment was regarded as a targeted dental examination that could result in dental intervention); control (C): no PDA; outcome (O): PJI. We included randomized and non-randomized studies with proper control of which full reports were published before the day of the last search update (i.e., 10th September 2024). No language barrier was set. Animal studies, case reports, case series, conference abstracts and reviews were excluded.
Search strategy
The search was conducted using MEDLINE (including MeSH terms), EMBASE, Scopus, Web of Science and Google Scholar. Appropriate sensitive search filters were used to exclude animal studies. The studies were screened to detect appropriate titles and abstracts. For the search in MEDLINE, we implemented the following key words (full strings are available on request): (dental screening OR oral health OR dental assessment OR dental clearance OR oral care OR dental care OR dental sanation OR oral sanation OR dental health OR dental intervention) AND (hip replacement OR hip arthroplasty OR knee replacement OR knee arthroplasty OR arthroplasty OR orthopaedic surgery OR total knee replacement OR total hip replacement OR total joint replacement).
Study selection and data collection process
Articles were pre-qualified and added to the Mendeley database, and were then evaluated using titles and abstracts. Two independent investigators screened the articles (M.M. and M.K.). A study was processed further if both investigators agreed to include the paper for the review. Any disagreements were resolved by the third investigator (Z.P.). Full-text assessments were carried out with the same rigor.
Data items
Extracted data contained the main author’s name, year of publication, population size, population demographics, type of procedure, description of dental care and outcomes. When necessary, attempts were made to contact authors for missing data.
Risk of bias assessment
Risk-of-bias assessments were conducted in duplicate (M.M. and M.K.) using a custom data collection form. Disagreements were resolved by the third investigator (Z.P.). Risk of bias was assessed using the Risk of Bias in Non-Randomized Studies of Interventions tool for nonrandomized studies (ROBINS-I). We determined the overall ROBINS-I for each trial based on the highest risk attributed to any one domain.
Effect measures
The principal summary measure used for the quantitative analysis was the odds ratio (OR) with 95% confidence interval (95% CI) for the PDA to reduce the frequency of postoperative prosthetic joint infection.
Synthesis methods
We pooled the outcomes by random-effects meta-analysis and Bayesian meta-analysis. Assessment of heterogeneity between studies was conducted using the χ2 test and we assessed the total variance due to heterogeneity rather than sampling error by I2. Bayesian meta-analysis was carried out with a weakly informative normal prior: (effect prior: mean = 0, SD = 2.82 and heterogeneity prior: half-normal with scale 0.5) [13]. Additionally, we conducted trial sequential analysis (TSA) using the random effects model for the primary outcome. For the TSA, we used a statistical significance level of 5%, a power of 80% and a relative risk reduction of 10% to represent a clinically important difference. We assessed the certainty of evidence for each outcome using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach.
RevMan Version 5.4 was used for traditional meta-analysis and R (bayesmeta package) was used for the Bayesian approach to the results. We performed TSA analyses using Trial Sequential Analysis version 0.9.5.10 beta (Copenhagen Trial Unit, Centre for Clinical Intervention Research, Rigshospitalet, Copenhagen, Denmark, www.ctu.dk/tsa).
RESULTS
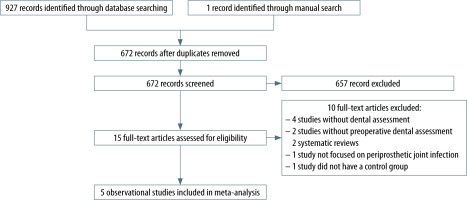
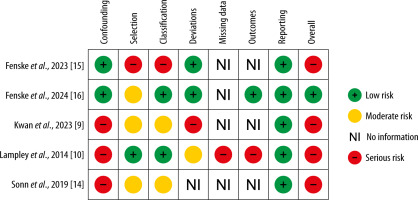
After performing a systematic search (Figure 1), only 5 single-centre, observational cohort studies were deemed eligible for inclusion [9, 10, 14–16]. There were 3 studies with prospectively designed PDA [10, 15, 16] and 2 studies with retrospectively gathered data about any PDA [9, 14]. By using the ROBINS-I tool, one study [16] was considered to be at “moderate” risk of bias, whereas the remaining four studies were rated as having a “serious” risk of bias (Figure 2).
In total, there were 23 175 patients, 12 324 of whom underwent PDA prior to the total joint repla-cement procedure (Table 1). In the group with dental assessment, 8.1% of patients had some form of dental intervention (i.e. dental extraction) [10, 14, 15]. The majority of patients, 58.8% (13 626/23 175), underwent a total knee arthroplasty procedure, whereas 37.7% (8747/23 175) underwent total hip arthroplasty and 1.2% (285/23 175) had a sledge prosthesis inserted. The studies differed in terms of PJI follow-up (within 4 weeks, before 90 days, after 90 days and within 1 year after surgery). The rate of PJI varied between 0.3% and 1.8% in the dental assessment group, whereas in the control group it varied from 0.2% to 2.4%.
TABLE 1
Summary of included studies
| Author (year) | Design | Population | Dental assessment description | Outcome definition | Intervention group (PJI/total) | Control group (PJI/total) | Conclusion |
|---|---|---|---|---|---|---|---|
| Lampley (2014) [10] | Single-centre Prospective cohort study with retrospective control group | Elective endoprosthesis + hip fractures | Patients were systematically evaluated by a dentist; if necessary, patients underwent dental treatment prior to the procedure | PJI within the first year after surgery | 6/356 (1.7%) | 4/161 (2.5%) | “The perceived need for routine preoperative dental screening for all hip and knee arthroplasty patients should be reassessed” |
| Sonn (2019) [14] | Single-centre Retrospective cohort study | Elective endoprosthesis | Preoperative dental evaluation that was available in patient’s medical records | PJI with follow-up longer than 90 days | 31/1685 (1.8%) | 3/328 (0.9%) | “Findings suggest that routine formal dental clearance for all TJA patients may not be necessary” |
| Fenske (2023) [15] | Single-centre Prospective cohort study with retrospective control group | Primary total joint arthroplasty | Patients were examined either by a dentist or by an instructed surgeon; if necessary, patients underwent dental treatment prior to a procedure | PJI within first 4 weeks after surgery | 4/402 (1.0%) | 6/375 (1.6%) | “The interventions in terms of oral screenings and need-based interventions thus did not lead to significant changes in the infection rates” |
| Kwan (2023) [9] | Single-centre Retrospective cohort study | Primary total joint arthroplasty | Preoperative dental clearance that was available in patient’s medical records | PJI with follow-up shorter than 90 days | 26/8654 (0.3%) | 21/8654 (0.2%) | “Eliminating dental clearance from routine preoperative clearance does not appear to increase the rates of acute PJIs” |
| Fenske (2024) [16] | Single-centre Prospective cohort study with retrospective control group | Primary and elective endoprosthesis | Specialized dentists performed a full dental examination and organized need-oriented therapy based on the risk classification system | PJI within the first month after surgery | 10/1227 (0.8%) | 24/1333 (1.8%) | “Dental referral using a standardized form can reduce the prevalence of early PJI. Accordingly, orthopedists and dentists should collaborate in this practical way” |
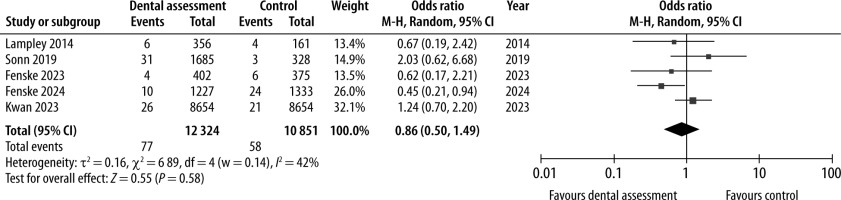
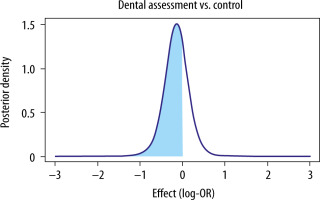
Random-effect meta-analysis (Figure 3) revealed no significant effect of PDA versus no PDA on the frequency of PJI (OR 0.86, 95% CI: 0.50–1.49; I2 = 42%). Bayesian analysis (Figure 4) showed that there is 69.1% posterior probability that PDA may reduce the risk of PJI. TSA showed that no optimal information size was reached to draw any definitive conclusions.
FIGURE 4
Effect of preoperative dental assessment for the reduction of periprosthetic joint infection. Bayesian meta-analysis, weakly informative normal prior. Posterior probability of effect: 69.1%
For the PJI outcome, risk of bias and inconsistency of results were rated as “serious”; therefore, the certainty of evidence was graded “low”. Hence, the GRADE narrative summary was that there is insufficient evidence to support routine preoperative dental examination prior to TJA (Table 2). Due to the paucity of data and the limitations of the included studies, no secondary outcomes or subgroup analyses could be performed.
TABLE 2
Summary of findings
DISCUSSION
We conducted a meta-analysis to assess the consequences of PDA for the frequency of postoperative PJI. The overall findings of this meta-analysis show that there is insufficient evidence to support routine, PDA prior to TJA. From the theoretical standpoint, PDA should be focused on eliminating any potential foci of infection that occur in the oral cavity and could potentially spread to the newly implanted endoprothesis [17]. These may be present in teeth with necrotic pulp, teeth after failed endo-dontic treatment, marginal and apical periodontitis, impacted teeth or teeth with difficult eruption, fragments of tooth roots left after extraction, complications after root apex resection, purulent cysts or bone inflammation. Hence, the preventive approach of PDA seems plausible, but the available data do not support this hypothesis. Moreover, a focus on preoperative dental procedures may inadvertently extend the waiting time for the primary joint replacement, a critical consideration from the patient’s perspective, as prompt intervention is vital for optimal functionality. Importantly, prolonged delays in joint replacement procedures can result in various complications, including thromboembolic events, contracture development, muscle atrophy, and osteoporosis [18, 19].
Although this meta-analysis included over 20 000 patients, the total incidence of PJI remained very low (0.58%) and was smaller than usually reported in the literature (1–2%) [2]. This, together with the fact that only a minority of PDAs (~8.1%) resulted in dental interventions that could possibly translate into a clinical benefit, indicates that the current data are not sufficiently powered to provide reliable answers about the effect of PDA on PJI. However, Bayesian analysis revealed a possible protective effect of PDA on PJI (posterior probability of effect = 69.1%). Nevertheless, it is very likely that the size of the effect, if present, is minimal, in either direction. This suggests that there is insufficient evidence to support performing a dental examination in each patient before surgery. One may obviously maintain that, regardless of the results of the analysis (and regardless of the surgical setting), a dental interview is important to obtain information about symptoms suggesting inflammation in the oral cavity and, if present, recommend proper treatment. In general, not only before surgery, the following are likely very important: awareness of oral health, prevention of diseases that may occur in the oral cavity, regular check-ups and dental examinations, which will make it possible to detect any acute or chronic pathological changes, and if they occur, implement appropriate treatment.
Strengths of this meta-analysis include: adhe-rence to the preregistered study’s protocol, implementation of the ROBINS-I tool, use of Bayesian analysis, TSA and assessment of evidence with the GRADE approach. Other strengths of this meta-analysis are that the studies included in this review were rather uniform in terms of included populations (elective TJA) and similarly defined PDAs. However, the studies differed in terms of duration of PJI follow-up, which may have led to underdetection of PJI in studies with shorter follow-up [9, 15]. Moreover, all of the studies utilized some form of retrospective data. The total frequency of PJI was lower than anticipated. Lastly, we were unable to pool predefined secondary outcomes or subgroups due to the paucity of available data.
Due to the above-mentioned considerations, we are unable to make a definitive recommendation for or against the routine use of PDA in patients undergoing TJA. The health care systems have to consider whether the effort, inconvenience and expenses associated with such programmes are justified in view of the lack of clear clinical evidence supporting their use. Further studies, presumably large, multicentre, randomized controlled trials, may be considered to address this issue, although the required population size seems prohibitive, as tens of thousands of patients would be required.
CONCLUSIONS
In patients undergoing TJA, it remains unknown whether PDA influences the occurrence of postope-rative PJI. There is insufficient evidence to support or refute the routine application of this intervention. Due to the infrequency of this complication and multiple factors influencing its occurrence, it is unlikely that higher quality data will be available. The health care systems will likely need to make decisions on continuation of such programmes on the basis of this limited amount of information. One option would be to perform such PDA selectively in patients with poor oral health who could afford the waiting time and financial burden associated with this intervention.